Preparation and Perseverance - Part 2
A Mindset of Perseverance
Chelsea Roman always knew that one day she’d face the decision to go on dialysis, and in September 2017 the time had come. Not that it was an easy – or happy – moment. Quite the opposite. But she’d spent her life getting her body, mind and spirit prepared. And she was ready. Read Part 1 of her story here.
Ahead of an undetermined but unavoidable appointment with kidney failure, Chelsea had done her research. She wanted to know about all the options and chose a transitional dialysis care program so she could learn the ins and outs of in-center, peritoneal dialysis (PD) and home hemodialysis (HHD).
“They really focused on my lifestyle,” she recalls. “They asked questions like ‘How many animals do you have? What is your daily routine like? Do you have room for storing supplies? Do you have access to water? Drainage?’ I wish more people had the opportunity to go through the transitional program because it changed my life.”
Properly educated, Chelsea had a choice to make. An avid traveler, she decided in-center wasn’t for her – too little freedom. She toyed with the idea of PD but didn’t like the thought of another surgery (having had four over 2014-2015) and she was concerned about using her hot tub.So, she set her sights on HHD and started training.
“I knew I was going to a home program the day I started. I didn’t know what to expect when I arrived,” Chelsea recounts. “I spoke to a specialist about my fears, and my fear was the needles. I was excited, but I was nervous. I wanted to feel better.”
After her first experience, she felt worse. The tech infiltrated Chelsea’s vein, and she went home in tears, and in lots of pain. But she wasn’t going to quit.
“They sent me home and I came back the next day,” remembers Chelsea. “I was persistent. They hooked me up again, and I cried through the needles, but after the machine started I said, ‘This isn’t too bad … this is ok, maybe I can do this.”‘ Before long, Chelsea would go from HHD rookie to full-blown rockstar.
She got past the needles and procedural stuff…
“I don’t mind poking myself, I don’t mind the prep work, I don’t mind cleaning my access. Medicine is something I’ve always been interested in anyway.”
She embraced her new HHD schedule and lifestyle.
“I dialyze 4 days a week. I feel great, I really do. I felt good right after the first treatment. I had heard you’d be wiped out and would go right to sleep and sleep until the next day – but that wasn’t the case.”
“My husband and I went to Maui in May 2018, and we took the machine. All the supplies were already there in our condo when we got there (Chelsea had ordered them ahead of time from her center). I dialyzed right in front of the ocean.”

She trained to do solo hemodialysis, for herself and her husband…
“I do my treatments by myself while (husband Mark) is at work. We have our nights back and our quality time back. I get off treatment, I make dinner … I have the energy and I can do things at night.”
“Because I’m able to do my treatment by myself, Mark has that freedom too. He doesn’t have to be worried and stressed out about it … When he sees me now, he sees ME – not me hooked up to a machine.”
“A woman read my story (in the newspaper) and volunteered to be my donor. It turned out she wasn’t a match for me … but she matched with someone, and just had her surgery in December 2018. Because she donated, she created a four-person donor chain. My story impacted four lives.”
“Deep breaths, relaxation, meditation are all things that help me while navigating dialysis multiple times on a weekly basis.”
Chelsea admits things aren’t always easy. It takes hard work and dedication to learn to administer dialysis at home, to yourself, by yourself. There are days when she doesn’t feel on top of the world, or completely in control. But she is also determined (a self-described Dialysis Warrior) and willing to do what it takes to keep ahead of her disease.
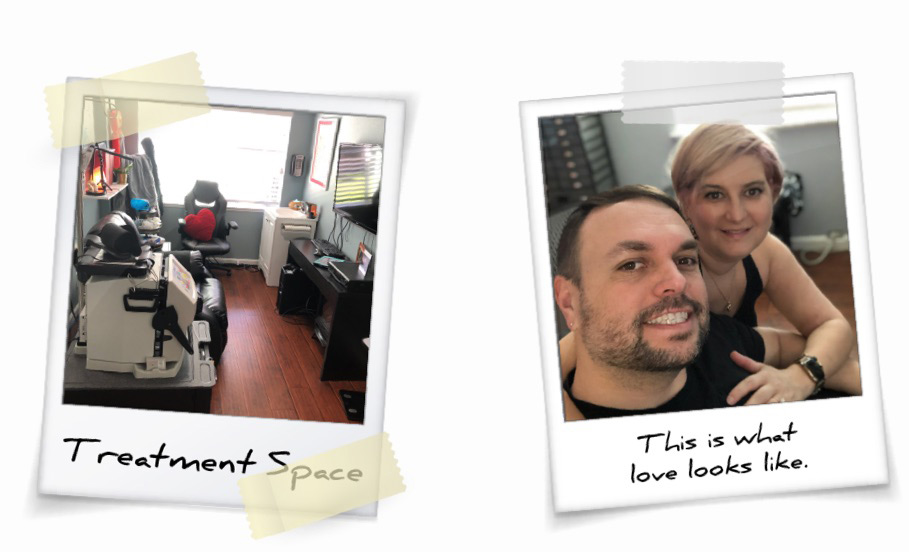
One of the biggest changes was transforming an existing sunroom into Chelsea’s “dialysis room.” In addition to her NxStage System One, it has a comfy chair, a TV, multiple drawers and cabinets and dispensers to keep supplies handy and clean, and even a sink for easy washing and cleaning up.
“It’s like my little dialysis clinic,” says Chelsea. “It was important for us because we wanted a space separate from the rest of the house where I could do dialysis. I wanted to be able to close it off when I wasn’t doing dialysis and I wanted it to be as comfortable as possible.”
While she waits and hopes for a transplant, Chelsea’s goals are simple. Stay healthy, stay happy, stay focused and educate as many as possible about the choices available to the many others who, like her, need dialysis to keep living.
“That’s my goal, to help people,” she says. “Because I think you can live a great life on dialysis. I believe you can do that, and I’m proof of it.”
Risks and Responsibilities
Risks Associated with Solo Home Hemodialysis Therapy
A qualified patient may dialyze alone, without a care partner present (solo home hemodialysis), provided the patient and physician agree that solo home hemodialysis is appropriate. Certain risks associated with hemodialysis treatment are increased when performing solo home hemodialysis because no one is present to help the patient respond to health emergencies. If patients experience needles coming out, blood loss, or very low blood pressure during solo home hemodialysis, they may lose consciousness or become physically unable to correct the health emergency. Losing consciousness or otherwise becoming impaired during any health emergency while alone could result in significant injury or death. Additional ancillary devices and training are required when performing solo home hemodialysis.






